Across dozens of specialties, thousands of providers, and complex payer contracts, Youlify operates at health-system scale.
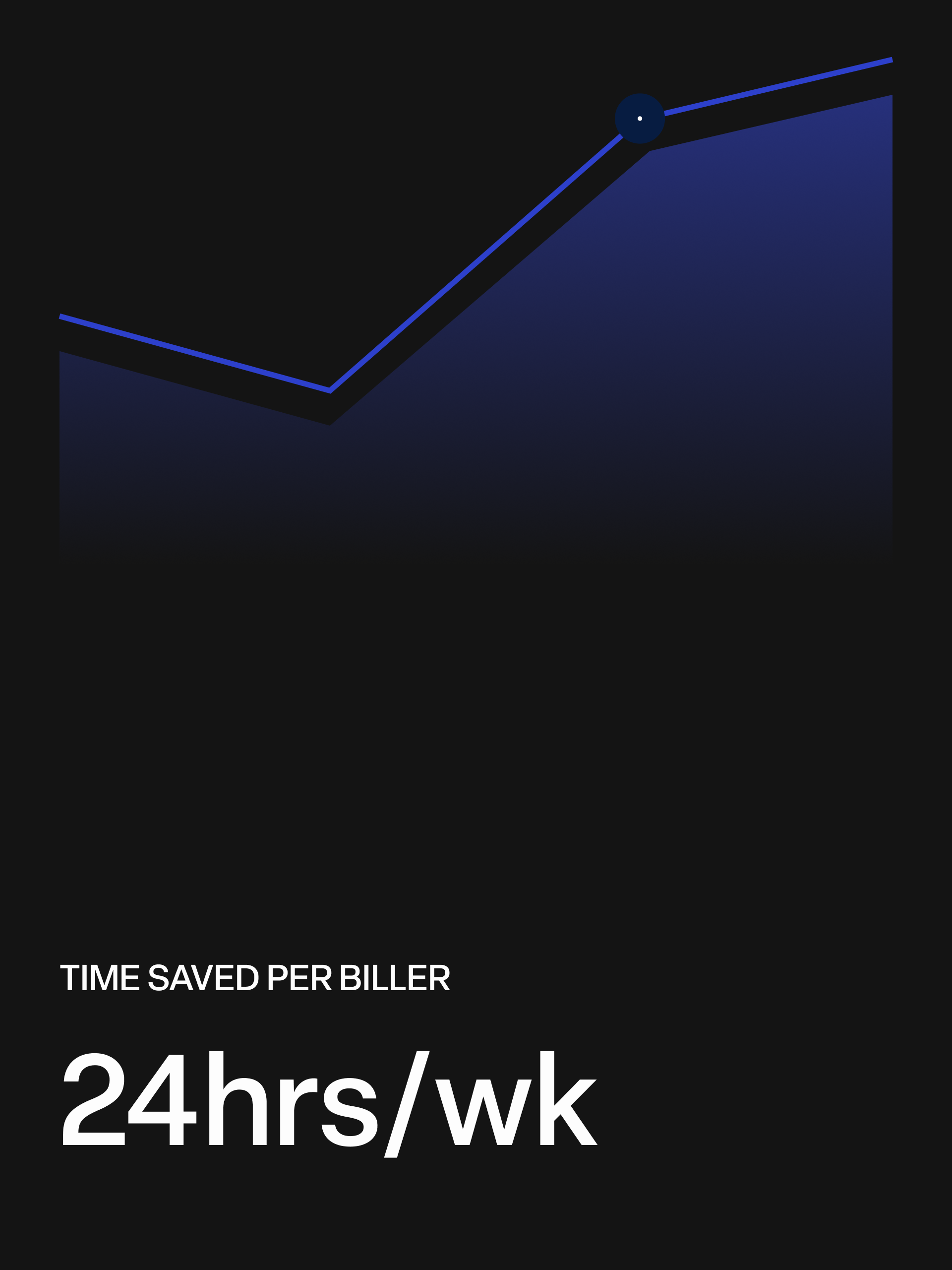
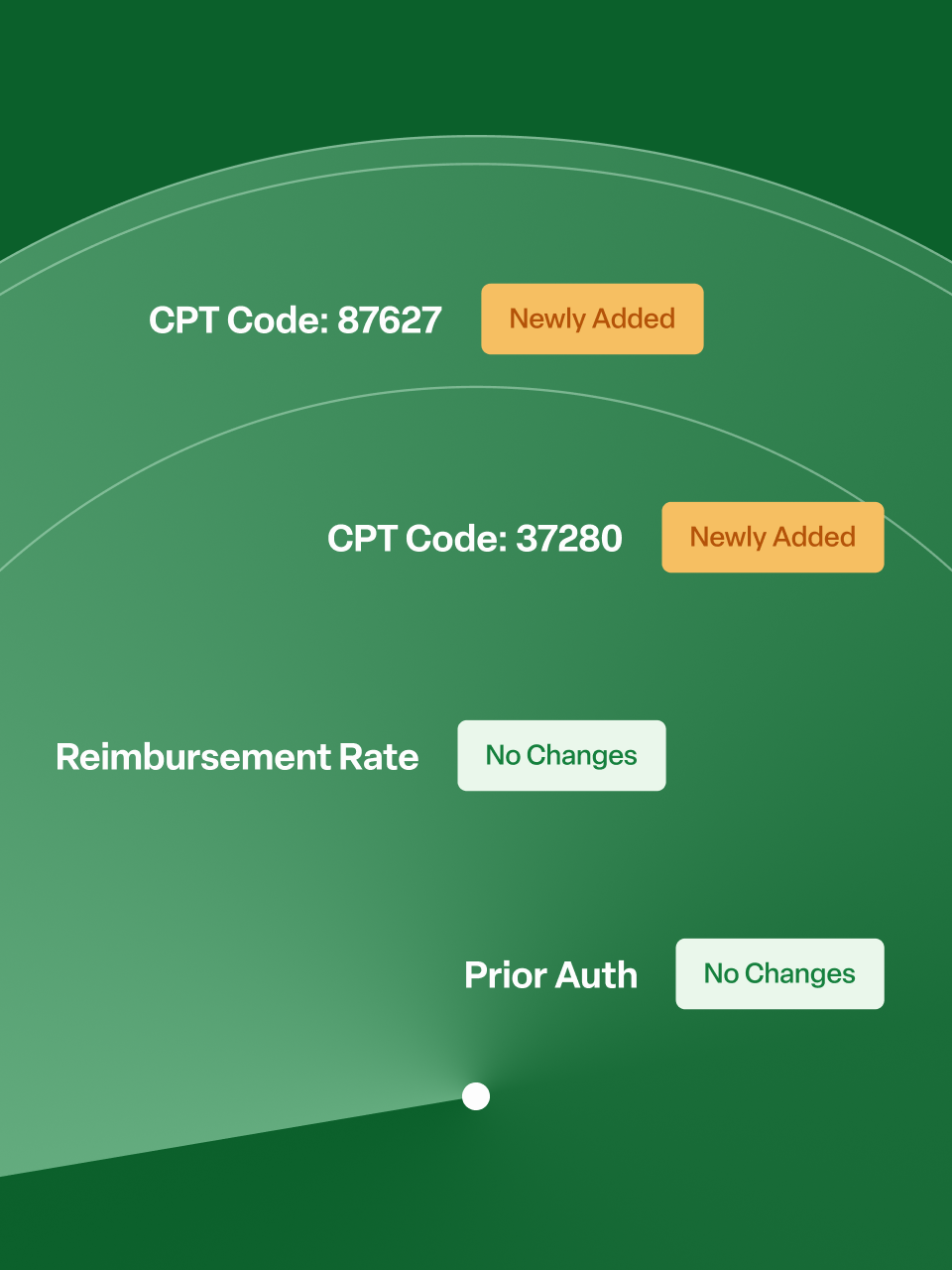
Our platform integrates into existing billing workflows, delivering real-time intelligence, bulk corrections, and automation of repetitive tasks, helping teams work more efficiently, prevent errors earlier, and focus their expertise on complex appeals, payer escalations, and revenue-critical strategy.